Abstract
Summary: Two patients with a cerebral embolism were evaluated by using both 99mTc-ethyl cysteinate dimer (ECD, or Bicisate) and 99mTc-hexamethylpropyleneamine oxime (HMPAO) single-photon emission computed tomography (SPECT). In one patient, 99mTc-ECD SPECT images revealed hypoactivity in a reflow hyperemic area where an infarct was seen later on CT scans. In another patient, a reperfused area showed hyperactivity on 99mTc-ECD SPECT without any abnormality on follow-up CT. 99mTc-ECD represents a potential agent with which to evaluate cerebral tissue viability in early reperfusion after ischemia.
Technetium-99m–labeled ethyl cysteinate dimer (ECD, or Bicisate) has been developed as a brain perfusion tracer for use with single-photon emission computed tomography (SPECT) (1). Early studies have shown that the distribution of 99mTc-ECD in the brain correlated with regional brain perfusion in healthy volunteers and in patients with chronic strokes (2–6). These investigators have also reported that 99mTc-ECD SPECT imaging failed to show reflow hyperemia and underestimated the flow abnormality in patients with subacute strokes as compared with 99mTc-hexamethylpropyleneamine oxime (HMPAO), N-isopropyl-p-[123I] iodoamphetamine (123I-IMP), and xenon-133 studies (4–6). To our knowledge, 99mTc-ECD SPECT imaging of reflow hyperemia within 24 hours after the onset of stroke has not yet been reported.
In this article, we describe two patients with early spontaneous reperfusion in cerebral embolism by comparing 99mTc-ECD SPECT with 99mTc-HMPAO SPECT imaging.
Case Reports
Case 1
Left-sided hemiparesis developed suddenly in a 54-year-old man with atrial fibrillation. A CT study of the brain 4 hours after onset of symptoms revealed no responsible lesion. 99mTc-HMPAO SPECT at 4.5 hours showed hypoactivity in the right frontal and temporal lobes (Fig 1A). Cerebral angiography revealed an embolic occlusion of the terminal portion of the right internal carotid artery. The patient was treated with steroids. Neither intraarterial nor intravenous thrombolytic therapy was used.
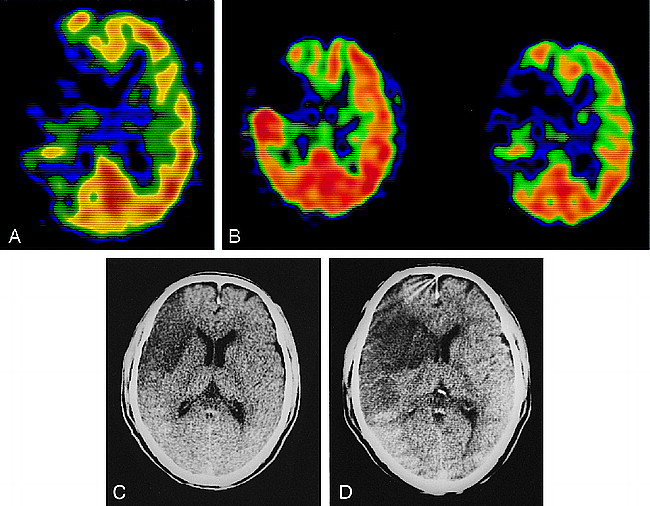
Case 1: 54-year-old man with atrial fibrillation and sudden onset of left-sided hemiparesis.
A, 99mTc-HMPAO SPECT image 4.5 hours after the onset of stroke shows hypoactivity in the right frontal and temporal lobes.
B, 99mTc-HMPAO SPECT image (left) obtained 12 hours after the initial study shows hyperactivity in the right temporal lobe; a 99mTc-ECD SPECT image (right) shows hypoactivity in the same area.
C, and D, CT scans after the SPECT study reveal a low-density area only in the right frontal lobe (C); 10 hours later, a partially hemorrhagic infarct has developed in the right temporal lobe (D).
Follow-up SPECT was performed 12 hours after the initial study. The first part of the follow-up study was begun 5 minutes after injection of 800 MBq of 99mTc-HMPAO and lasted 20 minutes. Immediately after the end of the 99mTc-HMPAO study, 950 MBq of 99mTc-ECD was injected. Five minutes later, the second SPECT study was carried out for 20 minutes. After reconstruction, the tomographic images from the first study were subtracted from the images of the second study, and the time differences in data acquisition were corrected to obtain 99mTc-ECD SPECT images. 99mTc-HMPAO and 99mTc-ECD SPECT images were produced independently by this subtraction technique.
Both sets of SPECT images depicted hypoactivity in the right frontal lobe. The 99mTc-HMPAO SPECT scans showed hyperactivity in the right temporal lobe, and the 99mTc-ECD SPECT scans showed hypoactivity in the same area (Fig 1B). Although a CT scan obtained after the SPECT study revealed a partial infarct in the right frontal lobe, low-density areas had not yet developed in the right temporal lobe (Fig 1C), and subsequent cerebral angiography showed partial recanalization of the lower trunk of the right middle cerebral artery (MCA). However, 10 hours later, the patient's motor functions rapidly deteriorated and a CT scan showed a partially hemorrhagic infarct in this area (Fig 1D).
Case 2
A 69-year-old man with atrial fibrillation was admitted with sudden onset of left hemiparesis. 99mTc-HMPAO SPECT was performed 7.5 hours after the onset of the symptoms and showed hypoactivity in the right parietal lobe (Fig 2A). Cerebral angiography showed an embolic occlusion of the central artery of the right MCA. Without intraarterial or intravenous thrombolytic therapy, his left hemiparesis resolved completely 10 hours after the onset of symptoms.
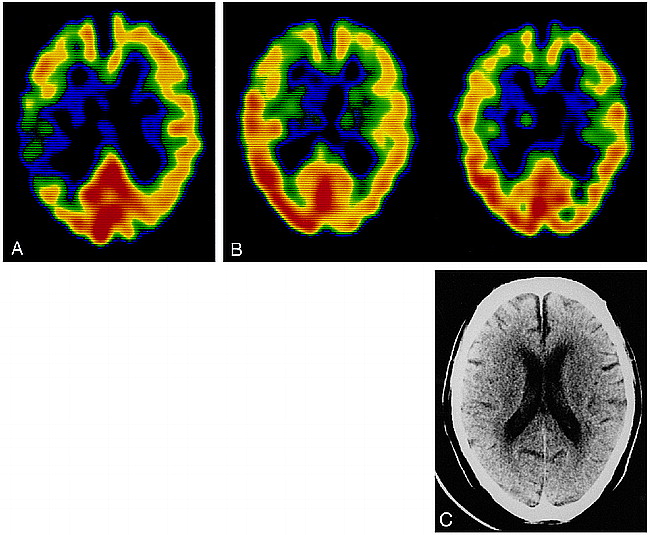
Case 2: 69-year-old man with atrial fibrillation and sudden onset of left-sided hemiparesis.
A, 99mTc-HMPAO SPECT image 7.5 hours after the onset of stroke shows hypoactivity in the right parietal lobe.
B, Both 99mTc-HMPAO (left) and 99mTc-ECD (right) SPECT images obtained 12 hours after the initial study depict hyperactivity in the right parietal lobe.
C, Follow-up CT scan does not show any abnormality.
Twelve hours after the initial SPECT study, we obtained 99mTc-HMPAO and 99mTc-ECD SPECT images using the same procedure as described for case 1. Both SPECT studies depicted hyperactivity in the right parietal lobe (Fig 2B). Subsequent cerebral angiography showed complete recanalization of the right MCA. A follow-up CT scan did not show any abnormality in the hyperactive area (Fig 2C).
Discussion
Follow-up 99mTc-HMPAO SPECT images obtained 12 hours after the initial study in our two patients showed focal hyperactivity indicative of reflow hyperemia. This reflow phenomenon is considered to be evidence of recanalization of occluded vessels due to spontaneous thrombolysis. Patients with embolic stroke often have reflow caused by early spontaneous thrombolysis in the acute stage.
99mTc-ECD is metabolized rapidly in the brain by a specific enzymatic pathway to a polar complex that is trapped in the brain (7). Because of this retention mechanism of 99mTc-ECD, hypofixation in reflow hyperemic areas in patients with subacute stroke may be due to either slow or absent deesterification caused by ischemic brain damage (4–6). In case 1, 99mTc-ECD SPECT images revealed hypoactivity in the reflow hyperemic area, whereas the CT scan obtained immediately after the SPECT study did not show low density. At follow-up CT 10 hours later, however, a partially hemorrhagic infarct had developed in this area of reflow hyperemia. This suggests that 99mTc-ECD SPECT may be able to predict whether an infarct will develop in patients with early reperfusion in ischemia before low density appears on CT scans. On the other hand, the findings in case 2 suggest that 99mTc-ECD SPECT may be able to depict focal hyperperfusion in areas without brain damage not only in focal seizures but also in reflow hyperemia, as Nakagawara et al (6) demonstrated in a patient with subacute stroke.
Conclusion
Although our observations are limited to two patients, they suggest that 99mTc-ECD is a potential agent with which to evaluate cerebral tissue viability in early reperfusion of ischemia. Additional studies are required to confirm these findings and speculations; however, the characteristics of 99mTc-ECD may be suitable for assessing the effects of fibrinolytic therapy using urokinase or tissue plasminogen activator in cerebral embolism, since these conditions often show signs of reflow hyperemia when therapy is successful. The greatest problem of fibrinolytic therapy has been reported to be hemorrhagic transformation, which may occur by early recanalization within a few hours after the insult in some patients and result in rapid deterioration of the patient's neurologic condition (8). Because reflow hyperemia in the nonviable neuronal tissue is considered to increase the risk of hemorrhagic transformation, 99mTc-ECD SPECT studies performed early after successful fibrinolytic therapy may predict neurologic exacerbation.
Footnotes
↵1 Address reprint requests to Kuniaki Ogasawara, MD, Department of Neurosurgery, Iwate Medical University, 19–1, Uchimaru, Morioka 020–8505, Japan.
- Received June 19, 1998.
- Copyright © American Society of Neuroradiology