Abstract
Summary: We describe and analyze the flow dynamics in replicas of a human anterior communicating artery aneurysm. The replicas were placed in a circuit of pulsating non-Newtonian fluid, and flows were adjusted to replicate human physiologic parameters. Individual slipstreams were opacified with isobaric dyes, and images were recorded on film and by CT/MR angiography. When flow in the afferent (internal carotid) and efferent (anterior and middle cerebral) arteries was bilaterally equal, slipstreams rarely entered the aneurysm. When flow in either the afferent or efferent vessels was not symmetrical, however, slipstreams entered the aneurysm neck, impinged upon the aneurysm dome, and swirled within the aneurysm. Unequal flow in carotid or cerebral systems may be necessary to direct pathologic, fluid slipstreams into an aneurysm.
In an innovative scientific article, Stehbens (1) described aneurysm formation and growth as a degenerative condition rather than a congenital phenomenon. We obtained a fresh cadaveric specimen of a lethal anterior communicating artery aneurysm and made accurate castings and reproductions of the aneurysm and surrounding arterial system. We then studied the flow dynamics in the replica-based models of the system, as well as the CT and MR angiographic correlates. We herein report the results of those experiments.
Technique
A 52-year-old woman died as a result of the rupture of an anterior communicating artery aneurysm (Fig 1). Under fluoroscopic control to ensure accurate vascular casting, catheterization was performed on the internal carotid arteries (ICAs) and epoxy resin was infused. After removal of the surrounding soft tissue, 12 clear elastic silicone replicas were created using the lost-wax technique, four of which were used for this particular experiment. All casts were measured at multiple points along the vessel with a digital dial-caliper exact to 0.001 inch (0.025 mm) to ensure accurate vascular reproduction. The resulting replicas, having been made from a human cadaveric source, provided highly realistic aneurysm geometry. Details of this process have been described previously (2). Although multiple replicas were made from the original vascular casting, all were accurate to within 1% of the original arterial system and all results were reproducible from each replica and each technique studied. The replicas were placed in a circuit of pulsatile non-Newtonian fluid with rheologic properties similar to blood (3). A blood pump (model 1421; Harvard Apparatus, South Natick, MA), cycling at one pulse per second, provided fluid flow. Flows were adjusted with a Square Wave Electromagnetic Flowmeter (Carolina Medical Electronics, King, NC) to replicate human physiologic flow profiles (ie, 40% forward flow during diastole), volumes (total bilateral ICA flow of 1200 mL/min), and velocities (approximately 80 cm/s at peak systole). The fluid slipstreams were opacified by injecting isobaric colored dyes through 30-gauge needles into the ICAs. Images were recorded on 35-mm film and on super VHS videotape at shutter speeds of 1/1000 second. For the first observations, all bilaterally equivalent vessels had the same flow rate: each ICA at 600 mL per minute, each middle cerebral artery (MCA) at 420 mL per minute (70% of ICA flow), and each anterior cerebral artery (ACA) at 180 mL per minute (30% of ICA flow). Flow was then asymmetrically reduced in each ICA, ACA, and MCA, respectively. With direct visualization, three observations were performed for each flow state, for a total of 21 observations. The replicas were then placed in a super-conducting magnet (GE Signa 1.5-T; GE Medical Systems, Milwaukee, WI), and MR angiograms were obtained using commercially standard 2D time-of-flight, 3D time-of-flight, and 3D phase-contrast pulse sequences during all described flow states. With MR angiography, one observation was performed for each flow state in each sequence, for a total of 21 observations. Next, the replicas were placed in a spiral CT scanner (GE Medical Systems) and CT angiograms were obtained using commercially standard shaded-surface display and maximum-intensity-projection algorithms also during all described flow states. With CT angiography, one observation was also performed for each flow state in each sequence, for a total of 14 observations. Analysis of slipstream flow during direct visualization, MR angiography, and CT angiography was conducted by consensus of all authors.
Angiogram of the left ICA, obtained before death, shows a multilobulated aneurysm at the junction of the right ACA and anterior communicating artery.
Results
Direct Visualization
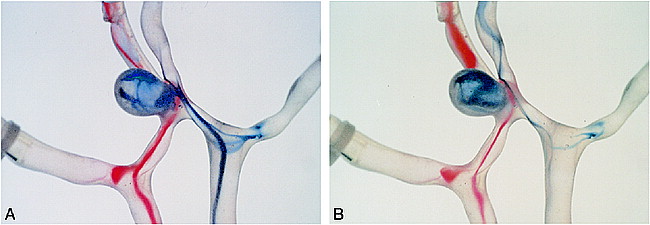
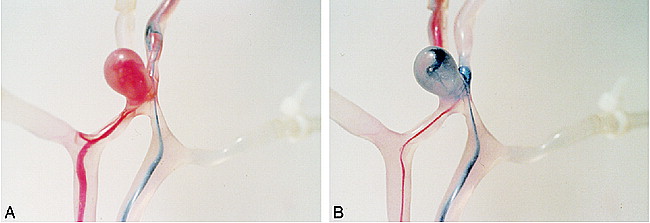
When flow rates in the afferent ICAs were equal, the opacified fluids slipstreams rarely entered the aneurysm (Fig 2). When flow was unequal between these vessels, rapid slipstreams entered the aneurysm neck and impinged upon the aneurysm dome, and the disturbed flow swirled within the aneurysm (Fig 3). This phenomenon was also observed when the efferent vessel flow was made asymmetrical; that is, when flow was reduced by partial vessel constriction of either an ACA or an MCA, disturbed slipstreams entered the aneurysm (Fig 4).
Symmetric flow between the afferent ICAs and the efferent ACAs and MCAs results in no significant slipstream entry into the anterior communicating artery aneurysm.
Asymmetric ICA flow. Images show opacified slipstreams entering the aneurysm neck and swirling within the aneurysm, with flow in the right ICA being twice that of flow in the left ICA. Although there is flow in both the ACAs and MCAs, for purposes of comparison with figure 4, individual slipstreams that primarily flow into the ACAs from the ICAs were opacified.
A, Image obtained 0.5 second before that shown in B.
B, Image obtained 0.5 second after that shown in A. Note the rapid run-off of dye within the right ICA compared with the left ICA.
Asymmetrical ACA flow.
A, Flow in the right ACA is reduced by 20% compared with flow in the left ACA, with slipstream entry into the aneurysm from the right ICA.
B, Flow in the left ACA is reduced by 20% compared with flow in the right ACA, with slipstream entry into the aneurysm from the left ICA.
MR Angiography
With symmetric bilateral flow and resultant lack of significant intra-aneurysmal flow, the aneurysm was difficult to perceive using MR angiography. Only when flow was asymmetrical between the ICAs or the ACAs/MCAs did the aneurysm become clearly visible, because intra-aneurysmal flow was then present.
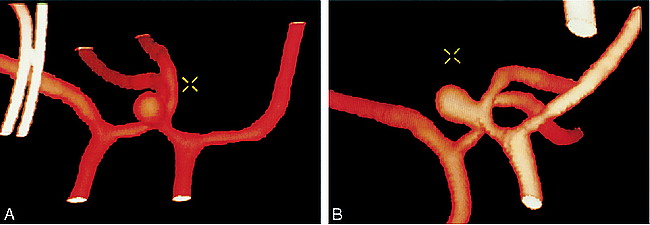
CT Angiography
Visualization of the aneurysm and the relationship between the aneurysm neck and parent vessels were clearly evident in all flow states. Three-dimensional projection analysis allowed rotation of the images for further anatomic clarification and even allowed creation of true stereoscopic image pairs (Fig 5).
Image pairs and further anatomic clarification.
A, CT angiogram of the anterior communicating artery replica and the surrounding vessels.
B, 3D projection and rotation showing excellent detail of the aneurysm neck and its relationship to the parent vessels.
Discussion
Cerebral aneurysms traditionally have been thought to be congenital in origin (4). Recent scientific articles have suggested that aneurysms are a degenerative condition (5–8). Although our observations are of only a single, yet highly realistic, anterior communicating artery aneurysm replica, the flow-dynamic analysis may support the degenerative theory. When flow was bilaterally equal between the ICAs, ACAs, and MCAs, opacified fluid slipstreams did not enter the aneurysm. This flow state should not result in aneurysm growth or rupture and is highly unlikely to result in aneurysm formation. When flow was bilaterally asymmetrical between either the afferent ICA or the efferent ACA or MCA, however, opacified fluid slipstreams entered the aneurysm. This flow state should result in aneurysm growth and possible eventual rupture and may be a factor in aneurysm formation. Asymmetrical flow of the afferent ICAs can be secondary to a fixed anatomic lesion, such as atherosclerotic carotid stenosis or, rarely, hypoplasia of the ICA (9, 10). In addition, temporary blood flow alterations may occur during changes in body position, such as head turning. Asymmetrical flow of the efferent arteries can be secondary to anatomic anomalies, such as hypoplasia of the A1 or P1 segments of the respective anterior or posterior cerebral arteries, or from atherosclerosis of these vessels (11, 12). Cerebral oxygen demand and resultant asymmetrical hemispheric blood flow may also contribute to asymmetric proximal cerebral artery flow. Further research is needed to determine which, if any, of these factors or other flow-altering processes may result in aneurysm development, growth, and rupture.
CT angiography easily depicted the aneurysm, its neck, and its relationship to the parent vessels, confirming the usefulness of CT angiography for anatomic aneurysm identification. MR angiography, which depends on flow, depicted only the aneurysm when intra-aneurysmal flow was present. Potentially, aneurysms may be missed by MR angiography if the patient's cerebral flow state while in the magnet results in lack of intra-aneurysmal flow. Future developments in MR angiographic resolution, however, may allow identification of individual flow slipstreams and provide more important in vivo physiologic data.
Acknowledgments
We gratefully acknowledge Dennis J. English for invaluable assistance in preparing the manuscript.
Footnotes
↵1 Address reprint requests to Charles W. Kerber, MD, Professor of Radiology and Neurosurgery, Department of Radiology, University of California, San Diego Medical Center, 200 West Arbor Drive, MC 8756, San Diego, CA 92103.
- Received August 21, 1998.
- Accepted after revision May 21, 1999.
- Copyright © American Society of Neuroradiology