January 2023
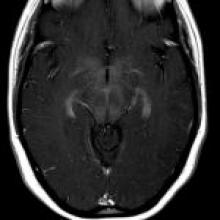
A 21-year-old woman presents with gait abnormality, recurrent falls, hand and lower extremity numbness, and subsequently altered mental status, encephalopathy, and fever. EMG reveals a sensory axonal polyneuropathy affecting mostly the upper limbs, while EEG is normal.